Decades of research have shown that healthcare accounts for only 10% to 20% of what defines a person’s health status and that social, behavioral, and genetic factors play a large role in determining overall health. Known as social determinants of health (SDOH), these other factors are the conditions of peoples’ social and physical environments that impact their health risks and outcomes, as well as their ability to access health services and adhere to recommended care. Examples of SDOH, which are often considered the underlying causes of medical conditions that require treatment include individual factors (like education, housing, and income), as well as neighborhood or community factors (like access to healthy foods or community support services and neighborhood safety or walkability).
Screening for SDOH and specific social risk factors, such as unstable housing, food insecurity, and lack of transportation, has become increasingly common in health care settings over the last few years, as appreciating the fuller context of the lives and lived experience of patients is fundamental to a patient-centered, whole-person approach to care. Knowing about social factors affecting patients’ lives can provide an opportunity to connect them with appropriate resources and modify care and treatment plans to account for a richer and more complex understanding of the patient’s own goals and circumstances. At the population level, understanding areas of need in the clinic and the community can inform advocacy and resource allocation, as well as provide data for focused, high-impact outreach in population health efforts.
The COVID-19 pandemic has further exacerbated health disparities, underscoring the importance of SDOH for better understanding how to address patient complexity and health equity via accessible telemedicine. Data collected during the pandemic indicates that interest and activity around SDOH remains high and points towards telehealth as one important and ongoing facilitator for SDOH efforts. At the outset of the pandemic, the volume of in-office primary care visits dropped precipitously across the United States and remained below prior levels through the end of 2020. In the absence of opportunities to engage with patients face-to-face, an increase in telehealth and virtual visits allowed providers to reach their patients (and vice versa) and maintain regular care.
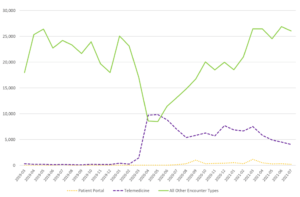
As in-office visits have returned closer to pre-pandemic levels, telehealth and virtual visit rates have slowed, but remain far above the levels seen at the start of 2020. In addition to clinical care, these shifts had a significant effect on SDOH screening and action. Across the OCHIN network of community health centers (CHCs), there was a substantial decline in overall SDOH screening activity captured in electronic health records (EHR) that corresponds with the drop in in-office visits starting in March of 2020. However, this was partially offset by a rapid increase in the proportion of SDOH screens being conducted in telehealth visits (Fig. 1) and, in both April and May of 2020, more SDOH screens were conducted via telemedicine (including virtual visits with video and those conducted by telephone only) than in all other encounter types combined. By October 2020, SDOH screening volumes were back up to pre-pandemic levels, but through mid-2021, telehealth visits have continued to account for roughly 15-20% of monthly SDOH screenings – up from effectively 0% at the start of 2020.
Figure 1. OCHIN Monthly SDOH Screens by Encounter Type
This data shows the importance of considering the implications of telehealth on collecting and acting on SDOH data. Many of the potential barriers
that affect working with SDOH in primary care in general are the same for telehealth, such as patient digital literacy, broadband connectivity, establishing trust, and maintaining relationships. Others are different or heightened for SDOH, often compounded by some of the very same social factors that those working with SDOH intend to address (e.g., financial strain, digital access, and lack of privacy).
The next articles in this three-part series will describe some of these factors affecting SDOH screening and action through telehealth and how they differ from the same considerations for in-office visits. There is plenty of reason to believe that virtual care will remain an important and growing component of primary care, such as that many patients preferred the convenience offered and not having to travel to office visits. In addition, payment parity policies for telehealth, a lifeline for many providers during the pandemic, have in some cases been extended or made permanent. Further, providers who made significant investments in telehealth and virtual care during the pandemic still have the necessary equipment and software, and now have over a year of real-world, stress-tested experience and workflow development behind it. While there are many challenges in this new telehealth-enabled landscape, we look forward to sharing success factors from experts in the field, as well as from OCHIN member clinics who have been navigating SDOH virtually through the pandemic. It’s our hope that these shared learnings and experience will help inform others’ efforts and continue the momentum around SDOH into the virtual future.
Questions or Comments? CONTACT US